Is “Bird Flu” H5N1 Spreading Among Diary Cows?

In recent months, there have been reports of highly pathogenic avian influenza H5N1 virus infecting dairy cows. This has raised concerns about the potential for human-to-human transmission and the possibility that H5N1 could spread among cattle populations.
The H5N1 Virus
Highly pathogenic avian influenza H5N1 is a subtype of the influenza A virus that primarily affects birds, but can also infect mammals, including humans. This virus was first detected in 1996 and has since caused outbreaks in many countries around the world.
The H5N1 virus is highly contagious among birds and can cause severe illness or death in infected poultry flocks. In addition to its impact on bird populations, this virus also poses a risk to human health. According to the World Health Organization (WHO), there have been over 860 reported cases of H5N1 infection in humans worldwide since 2003, resulting in 441 deaths.
The genetic makeup of H5N1 is characterized by a unique combination of genes from different influenza viruses. This has allowed the virus to evolve rapidly over time, making it difficult for humans and animals to develop immunity against it.
H5N1 in Diary Cows
In cattle, H5N1 infection typically causes respiratory symptoms such as coughing, sneezing, and nasal discharge. Infected animals may also exhibit fever, lethargy, and loss of appetite. In severe cases, the virus can cause pneumonia or other systemic illnesses that can lead to death.
Studies have shown that H5N1 can infect dairy cows and replicate within them, although the exact mechanisms of transmission are not yet fully understood. Research has also demonstrated that infected cattle can shed the virus in their milk or manure.
The H5N1 virus is highly infectious and can be transmitted through direct contact with an infected animal’s secretions, such as saliva, mucus, or feces. It can also be transmitted indirectly through contaminated surfaces, equipment, or feed.
The symptoms of H5N1 infection in dairy cows can vary depending on the severity of the illness. Mild cases may present with respiratory signs such as coughing, sneezing, and nasal discharge, while more severe infections can cause pneumonia or other systemic illnesses that can lead to death.
In some instances, infected cattle have shown no symptoms at all, making it essential for farmers and veterinarians to remain vigilant. The economic impact of H5N1 outbreaks on dairy farms cannot be overstated, as significant losses in milk production can occur.
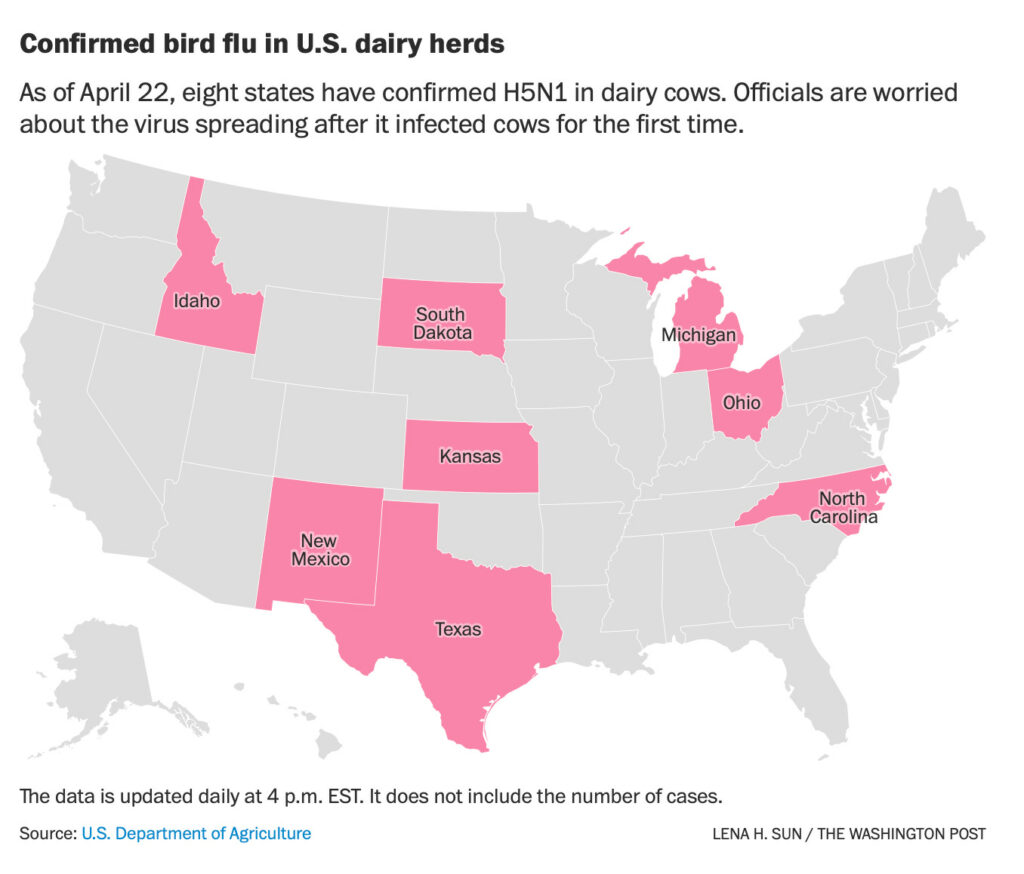
How Widespread Is the H5N1 Infection?
The extent to which H5N1 infection has spread among dairy cows is a topic of ongoing research and surveillance. While some cases have been reported, it appears that the virus is not as widespread as initially feared.
According to data from the U.S. Department of Agriculture (USDA), few tests from the respiratory tracts of infected cows have come back positive – and those that did showed there wasn’t a lot of virus present. However, at least some evidence suggests that H5N1 can occasionally get deep into the respiratory tracts of cows.
The main driver of infection among dairy cows appears to be milking parlors, where cows are strapped into milking machines. The amount of virus in the udders of infected cows is extremely high, making it easy for one cow’s infection to spread quickly throughout a herd.
“It can imagine that if such a cow is milked in a milking stall, even a few drops of milk remaining on the teat cup which is used to milk will then subsequently contaminate the teat of the next cow,” said Thijs Kuiken, a pathologist at Erasmus Medical Center. “So you can imagine very easily how, in the course of a few days, the virus could spread very fast among the cows being milked on that farm.”
This fits with other evidence: infections appear to be limited to lactating dairy cows, and the biggest milk producers. The fact that many non-lactating cattle in the same herds haven’t gotten sick suggests that H5N1 is not easily transmitted through direct contact or airborne means.
Still, it’s important for farmers to take precautions: washing hands and equipment after milking, disinfecting surfaces regularly, and keeping infected animals isolated.
Is The Milk Infected?
Can you get infected with H5N1 from drinking milk produced by cows that have contracted the virus?
Research has been ongoing to determine if all pasteurization techniques inactivate the virus. So far, findings are reassuring. Scientists at St. Jude Children’s Hospital in Memphis, Tenn., found genetic evidence of the virus in store-bought milk but were unable to grow live viruses from it, suggesting that pasteurization kills H5N1.
However, experts warn that raw milk – milk not subjected to heat treatment or sterilization – is a different story altogether. The concentration of virus present in infected cow’s milk is extremely high, making it possible for consumers who drink raw milk to ingest large doses of the virus.
The USDA has reported 34 outbreaks across nine states since late March, but crucial information about which dairy farms sold raw milk or if any producers had bird flu infections among their cows remains unknown. This lack of transparency raises concerns about potential risks associated with consuming raw milk during an outbreak.
If infected cows produce milk destined for the raw market, consumers could be exposed to a large dose of the virus. Concentrations as high as one billion virus particles per milliliter have been reported in some cases. Given these findings, experts like Kuiken believe that authorities should temporarily ban raw milk sales until the outbreak is under control.
While pasteurization appears effective against H5N1, more research and testing are needed to fully understand the risks associated with consuming milk from infected cows. In the meantime, consumers can take comfort in knowing that most commercial milk products have been heat-treated or sterilized, making them safer for consumption.
Are Farmers At Risk?
The recent outbreak of H5N1 avian influenza on dairy farms has raised concerns about the potential risks faced by farmers and farm workers who come into contact with infected animals. While there have been no confirmed human cases linked to this specific outbreak, some experts believe that it is possible for humans to contract the disease from cows.
One reason why more cases may not be reported is that many dairy farms are reluctant to test their employees or allow public health officials to conduct testing on site. This lack of cooperation makes it difficult to determine whether there have been any human infections linked to the outbreak.
Another factor that could contribute to underreporting is the mild nature of some symptoms experienced by farm workers who may be infected with H5N1. Conjunctivitis, or pink eye, can occur in people exposed to the virus and may not necessarily trigger a reportable case. This makes it important for public health officials to conduct thorough investigations at farms where cases have been reported.
Despite the lack of confirmed human cases linked to this outbreak, some experts believe that there could be undetected infections among farm workers or those who come into contact with them. Maria Van Kerkhove, acting head of the department of epidemic and pandemic preparedness at WHO, has called for studies to determine if antibodies to H5N1 are present in the blood of farm workers and others who have been exposed to infected animals.










