Why is rabies so dangerous and deadly?

Rabies is a viral disease that affects the central nervous system of mammals, including humans. It is caused by the rabies virus, which is typically transmitted through the saliva of an infected animal, most commonly through a bite.
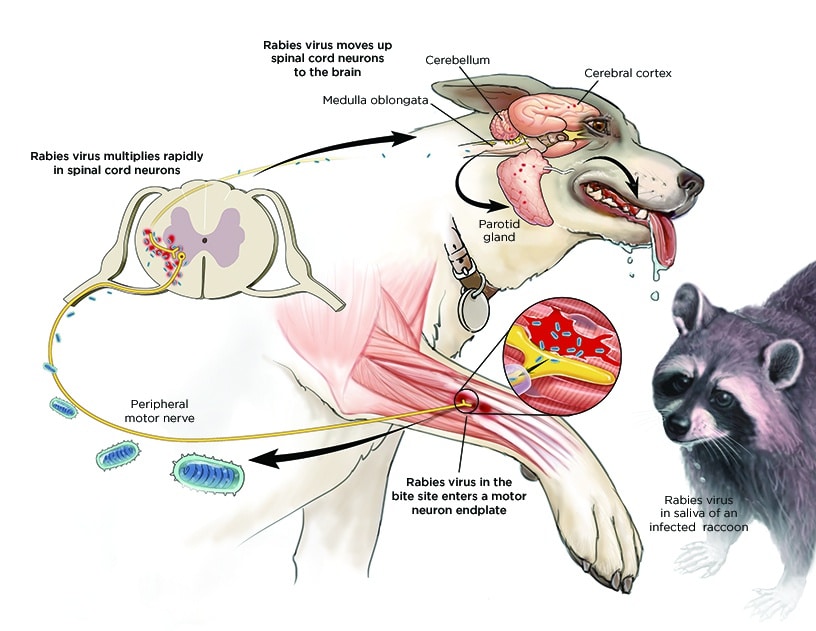
Once the virus enters the body, it travels along the peripheral nerves to the CNS, where it causes inflammation of the brain (encephalitis) and spinal cord.
The Rabies Virus
The rabies virus is a single-stranded RNA virus belonging to the Lyssavirus genus. It is a neurotropic virus, which means it has a strong affinity for nerve tissue. This affinity allows the virus to travel along peripheral nerves to the central nervous system (CNS), where it causes inflammation of the brain (encephalitis) and spinal cord.
The rabies virus is typically transmitted through the saliva of an infected animal, most commonly through a bite. However, the virus can also be transmitted through scratches, open wounds, or mucous membranes (such as the eyes, nose, or mouth) coming into contact with the saliva of an infected animal.
Once the virus enters the body, it replicates in muscle cells at the site of infection. From there, it travels along peripheral nerves to the CNS, where it causes inflammation and damage. The virus then spreads to other parts of the body, including the salivary glands, where it can be transmitted to other animals or humans through bites.
The rabies virus is typically not found in the bloodstream, which is why it is difficult to detect in the early stages of infection. However, once symptoms appear, the virus can be detected in the saliva, cerebrospinal fluid, or brain tissue of infected individuals.
There are several different strains of the rabies virus, which are classified into different genotypes based on their genetic sequences. These genotypes are associated with different reservoir species, or species in which the virus is commonly found. For example, genotype 1 is associated with domestic dogs and wild canids (such as foxes and wolves), while genotype 2 is associated with bats.
The Symptoms Of Rabies In Animals
Rabies is primarily a disease of mammals, and any mammal can be infected with the rabies virus. The symptoms of rabies in animals can vary widely, depending on the species and the stage of the disease.
Early Symptoms
In the early stages of rabies infection, animals may exhibit nonspecific symptoms, such as fever, lethargy, and decreased appetite. These symptoms can be easily overlooked, as they are similar to those of many other diseases.
Furious Form
As the disease progresses, animals may develop one of two forms of rabies: the furious form or the paralytic form. In the furious form, animals become highly agitated and aggressive. They may exhibit unusual behavior, such as biting at objects, attacking people or other animals, and making strange vocalizations.
Paralytic Form of Rabies
In the paralytic form of rabies, animals become weak and paralyzed. They may have difficulty walking or standing, and their movements may become stiff and jerky. They may also have difficulty swallowing, leading to excessive drooling and foaming at the mouth.
End Stage
In the end stage of rabies, animals become comatose and eventually die. The time from the onset of symptoms to death can vary widely, depending on the species and the individual animal.
Animals with rabies can transmit the virus to humans through bites or scratches. However, it is important to note that not all animals with rabies exhibit aggressive behavior. Some animals may appear calm and friendly, even as they are infected with the virus.
The Symptoms Of Rabies In Humans
The symptoms of rabies in human typically appear within a few weeks to several months after exposure to the virus. Initial symptoms may include fever, headache, and general weakness or discomfort. However, as the disease progresses, more severe symptoms emerge, and they are often fatal.
One of the hallmark symptoms of rabies is hydrophobia, an irrational fear of water. This symptom is due to the virus’s effect on the brain, particularly the part of the brain that controls swallowing. As the disease progresses, patients may experience difficulty swallowing, which is exacerbated by the fear of water. This fear of water can be so severe that even the sight or sound of water can trigger a violent reaction.
Other symptoms of rabies include hallucinations, confusion, and agitation. This is due to the virus’s effect on the brain, which can cause delirium and psychosis. Patients may also experience seizures, which can be severe and life-threatening. In some cases, patients may experience paralysis, particularly in the muscles of the face and throat, which can lead to difficulty breathing and swallowing.
As the disease progresses, patients may fall into a coma, and death usually occurs within a few days to weeks after the onset of symptoms. Once symptoms appear, rabies is almost always fatal.
The Importance of Vaccination
Rabies is a preventable disease, and vaccination is the most effective way to prevent infection. The most effective way to prevent rabies is through vaccination. In many countries, including the United States and Canada, vaccination programs for domestic animals have been successful in reducing the number of rabies cases. However, in many developing countries, access to vaccines and preventive measures is limited, leading to ongoing outbreaks of the disease.
In addition to vaccination, other preventive measures include avoiding contact with wild or stray animals, especially those that are behaving strangely or aggressively. In the event of a bite or scratch from a potentially rabid animal, immediate medical attention is crucial. Post-exposure prophylaxis (PEP) can prevent the development of rabies in people who have been exposed to the virus.

Jeanna Ann Giese-Frassetto: First Known Rabies Survivor Without Vaccination
There is a remarkable and unique case of rabies survival: the story of Jeanna Ann Giese-Frassetto. In 2004, she became the first known person to survive rabies without prior vaccination.
Jeanna was a 15-year-old girl from Wisconsin who was bitten by a bat while attending church. Initially, the bite was dismissed as insignificant, but soon Jeanna began experiencing symptoms that were later diagnosed as rabies. Her case was exceptional because, by the time she sought medical attention, the virus had already reached her central nervous system, where it usually becomes untreatable.
Jeanna’s treatment was experimental and involved inducing a coma to prevent her body from fighting the infection, allowing her immune system to develop antibodies to fight the rabies virus. This method, known as the Milwaukee protocol, was developed by Dr. Rodney Willoughby, who was treating Jeanna. The protocol also included aggressive antiviral drug therapy and supportive care.
After a prolonged period of induced coma and extensive medical intervention, Jeanna eventually recovered from the rabies infection. Her story provided hope and inspiration to those working in the field of rabies research and treatment.
Despite this extraordinary case, the Milwaukee protocol has not been widely adopted due to its complexity, potential risks, and lack of definitive evidence of its effectiveness. However, Jeanna’s survival has contributed to our understanding of rabies and the potential for novel treatments.
The Global Impact of Rabies
Rabies is a viral disease that has a significant global impact, affecting both human and animal populations. Despite being entirely preventable, it continues to cause thousands of deaths every year, mainly in developing countries where access to preventive measures and medical care is limited.
Human Toll
The World Health Organization (WHO) estimates that rabies causes approximately 59,000 human deaths annually, with the majority of these occurring in Africa and Asia. The disease is particularly prevalent in rural areas, where people are more likely to come into contact with infected animals, such as dogs, cats, and wildlife.
Rabies is a particularly cruel disease, as its symptoms are excruciating and often irreversible. Once symptoms develop, which typically occurs within one to three months after exposure, the disease is almost always fatal. The progression of rabies is marked by anxiety, confusion, agitation, and ultimately paralysis, coma, and death. The victim often becomes afraid of water (hydrophobia), making it challenging to administer life-saving treatments.
Economic Impact
The economic impact of rabies is significant, with an estimated $8.6 billion spent annually on rabies prevention and control measures worldwide. These costs include vaccination programs for both humans and animals, post-exposure prophylaxis (PEP), and the treatment of rabies cases.
In many developing countries, the cost of rabies treatment is beyond the means of most individuals and communities. This often leads to underreporting of rabies cases and an insufficient number of people receiving post-exposure prophylaxis, contributing to the high mortality rate associated with the disease.
Animal Toll
Rabies also takes a toll on animal populations, particularly in regions where the disease is endemic. Domestic animals, such as dogs, cats, and livestock, can become infected with the rabies virus, leading to the spread of the disease to humans and other animals.
Wildlife is also affected by rabies, with species such as raccoons, skunks, and foxes acting as reservoirs for the virus. This can lead to outbreaks of rabies in domestic animal populations, as well as increased risk of transmission to humans.










